According to Dr. Mark Hyman, 95 percent of all illness is caused or worsened by stress!
There are 2 branches of the nervous system: sympathetic and parasympathetic. The sympathetic branch is known as the “fight or flight” system (some people are now adding “freeze”), and the parasympathetic branch, “rest and digest”. It is important to have these two branches of the nervous system so we can appropriately respond to our environment. The problem most people deal with, is the stress of life becoming chronic stress, constantly activating that sympathetic fight or flight response, versus the rest and digest response. Dr. Neil Neimark, MD writes a comprehensive description of the fight or flight response and its effect on the body.
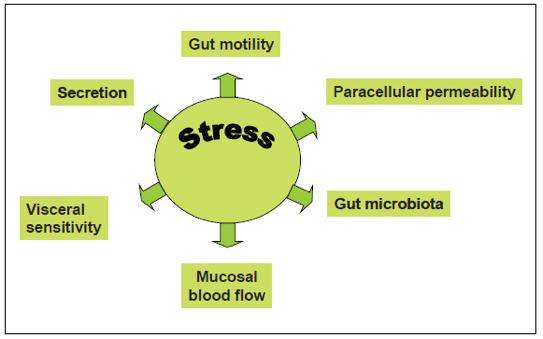
Essentially, our response to the environment gets converted into molecules. The “molecules of emotion” or “information substances” circulate throughout our body and can affect our mind, emotions, immune system and digestion. Cortisol is a hormone produced by the adrenal glands in response to a stressor, and epinephrine/norepinephrine commonly known as adrenaline/noradrenaline, are neurotransmitters released from the adrenal gland. Adrenaline is the quick response, whereas cortisol is slightly slower in its release. Once they reach their destination, they have an effect, and chronic exposure to these stress-induced substances can lead to chronic degeneration.
The word stress is usually associated with psychological distress. The body also experiences stress from physiologic triggers: skipping meals and letting blood sugar drop, extreme exercise, lack of sleep, and fighting chronic infections- all of these things can also raise cortisol levels.