Why do we need functional medicine?
- Our society is experiencing a sharp increase in the number of people who suffer from complex, chronic diseases, such as diabetes, heart disease, cancer, mental illness, and autoimmune disorders like rheumatoid arthritis and fibromyalgia.
- The system of medicine practiced by most physicians is oriented toward acute care, the diagnosis and treatment of trauma or illness that is of short duration and in need of urgent care, such as appendicitis or a broken leg. Physicians apply specific, prescribed treatments such as drugs or surgery that aim to treat the immediate problem or symptom.
- Unfortunately, the acute-care approach to medicine lacks the proper methodology and tools for preventing and treating complex, chronic disease. In most cases it does not take into account the unique genetic makeup of each individual or factors such as environmental exposures to toxins and the aspects of today’s lifestyle that have a direct influence on the rise in chronic disease in modern Western society.
- There’s a huge gap between research and the way doctors practice. The gap between emerging research in basic sciences and integration into medical practice is enormous—as long as 50 years— particularly in the area of complex, chronic illness. Functional medicine’s aim is to evaluate, assess, and carefully enfold emerging research in a practical, efficient, and safe manner.
- Most physicians are not adequately trained to assess the underlying causes of complex, chronic disease and to apply strategies such as nutrition, diet, and exercise to both treat and prevent these illnesses in their patients.” (1)
How is functional medicine different?

Conventional treatment options for autoimmune disease are fairly standardized worldwide:
“Currently there are no cures for autoimmune diseases, although there is a wide range of treatment options, which depend on the stage and type of autoimmune disease. The main aims of treatments for autoimmune diseases are to relieve symptoms, minimise organ and tissue damage and preserve organ function. Treatment options, usually under specialist supervision, include one or more of:
- Replacement of end organ functions (such as insulin in diabetes and thyroxine in autoimmune thyroid disease)
- Non-steroidal anti-inflammatory medications (NSAIDS)
- Corticosteroid anti-inflammatory medications (such as Prednisolone)
- Immunosuppressive medications
- Therapeutic monoclonals (such as TNF inhibitors)
- Immunoglobulin replacement therapy” (2)
Many of these drugs have serious adverse effects. Even something as seemingly benign as NSAIDS (non-steroidal anti-inflammatory drugs like Ibuprofen and Acetaminophen) are actually contraindicated, especially in people with autoimmune diseases like IBD (“NSAIDs have some undesirable and adverse effect, such as ulcers, kidney injury, and bleeding in the gastrointestinal tract”). (3) Prednisone is not a long-term solution, causing mood swings, weight gain, and bone-density loss, and such immunosuppressants and TNF inhibitors — where TNF is considered “the master pro-inflammatory cytokine”(3) — can leave a patient open to increased incidence of other diseases due to the suppression of white blood cell activity and other factors.
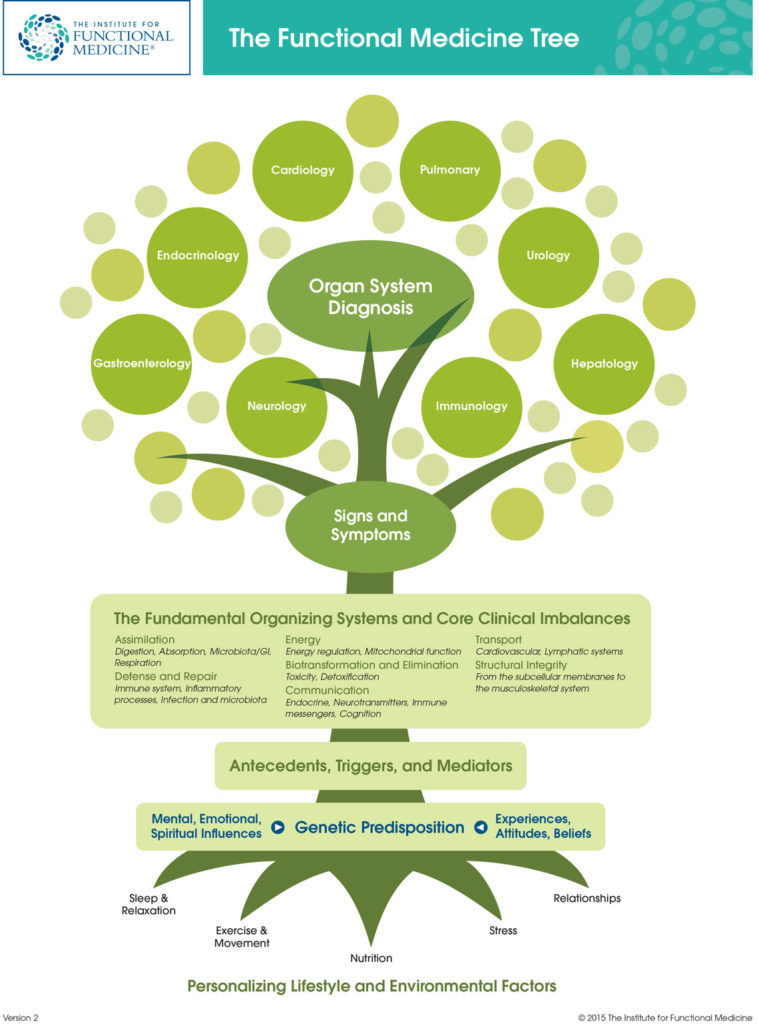
The functional medicine approach, by contrast, looks at root causes. The Institute for Functional Medicine uses a tree symbol to show the distinction: where functional medicine is in the bottom half of the graphic, symbolizing the attributes they study, looking at root causes for disease, the conventional approach is represented by the top half of the graphic, the different branches and specialties of conventional western medicine, which thinks of these areas as being distinct from one another, instead of as part of one integrated system:
Many functional medicine practitioners came up through the system as conventional practitioners themselves, and then, when they themselves got ill and found unsatisfactory answers in the standard approach, took a new approach with functional medicine: as Dr. Mark Hyman says, “In conventional medicine, most of us were taught to diagnose disease by symptoms, NOT by their underlying cause…conventional strategies like powerful immune-suppressing medication fail to address the underlying cause. That’s like taking a lot of aspirin while you are standing on a tack. The treatment is not to take more aspirin or a strong immune suppressant; it is to remove the tack.” (4)
Here is the functional medicine approach as outlined, again, by the Institute for Functional Medicine, is as follows:
Functional medicine involves understanding the origins, prevention, and treatment of complex, chronic disease. Hallmarks of a functional medicine approach include:
- Patient-centered care. The focus of functional medicine is on patient-centered care, promoting health as a positive vitality, beyond just the absence of disease. By listening to the patient and learning his or her story, the practitioner brings the patient into the discovery process and tailors treatments that address the individual’s unique needs.
- An integrative, science-based healthcare approach. Functional medicine practitioners look “upstream” to consider the complex web of interactions in the patient’s history, physiology, and lifestyle that can lead to illness. The unique genetic makeup of each patient is considered, along with both internal (mind, body, and spirit) and external (physical and social environment) factors that affect total functioning.
- Integrating best medical practices. Functional medicine integrates traditional Western medical practices with what are sometimes considered “alternative” or “integrative” medicine, creating a focus on prevention through nutrition, diet, and exercise; use of the latest laboratory testing and other diagnostic techniques; and prescribed combinations of drugs and/or botanical medicines, supplements, therapeutic diets, detoxification programs, or stress-management techniques. (1)
To helps you discuss the subject with others, here’s a handout from the Institute of Functional Medicine on what functional medicine is, why we need it, and how it’s different.
- “The Functional Medicine Approach” © 2008 The Institute of Functional Medicine. Used by permission. Visit www.functionalmedicine.org for more information.
- Australasian Society of Clinical Immunology and Allergy (ASCIA), “Autoimmune diseases”, www.allergy.org.au 2016.
- “Drugs for Autoimmune Inflammatory Diseases: From Small Molecule Compounds to Anti-TNF Biologics” by Ping Li, Ying Zheng, and Xin Chen in NCBI NIH Frontiers in Pharmacology, July 2017.
- Dr. Mark Hyman, “10 Steps to Reverse Autoimmune Disease, “ blog post September 4, 2015.


