This phase of the 5R approach involves repair of the damaged GI tract barrier. Considering all of the insults that are put upon the GI tract on a regular basis, it is not surprising that it may need extra help. The GI tract has to be thin enough to allow for an exchange of nutrients from our diet to be quickly and easily absorbed. It also has to play the role of keeping damaging things out. The outer lining of the GI tract is only 1 layer of cells thick. There is a protective mucus layer over these cells and a connective tissue layer beneath these cells. This thin layer leaves the GI tract a vulnerable place, prone to injury.
What is leaky gut?
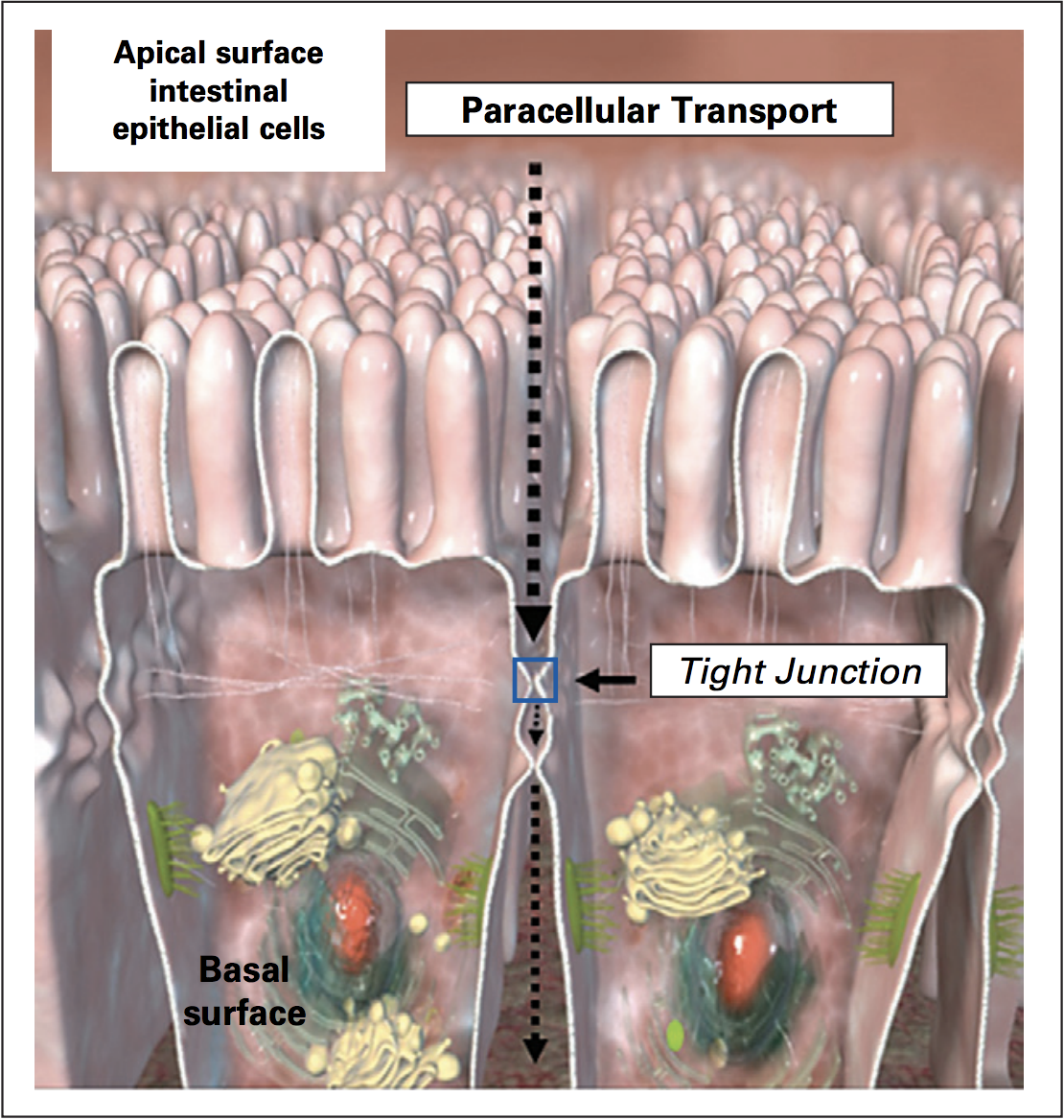
(Picture reference)
The picture above is a cross section of two intestinal cells beside each other. The cells are lined up next to each other like a sheet that covers the entire gut tube. Between the cells are tight junctions, which serve as gates allowing a certain amount of things to pass. This opening and closing of the tight junctions is considered a normal physiological process. It helps to flush out bacteria and bacterial toxins. When these tight junctions remain open for prolonged periods of time, more can pass through than what is typically allowed and this is where problems can start. This is known as intestinal permeability, or “leaky gut”, where things “leak” through when they aren’t supposed to. Leaky gut happens when the regulatory mechanism is impaired.1
In addition to leaky gut, the cells themselves can become damaged, which decreases their function of being able to absorb nutrients.
The central role of gut permeability or “leaky gut”
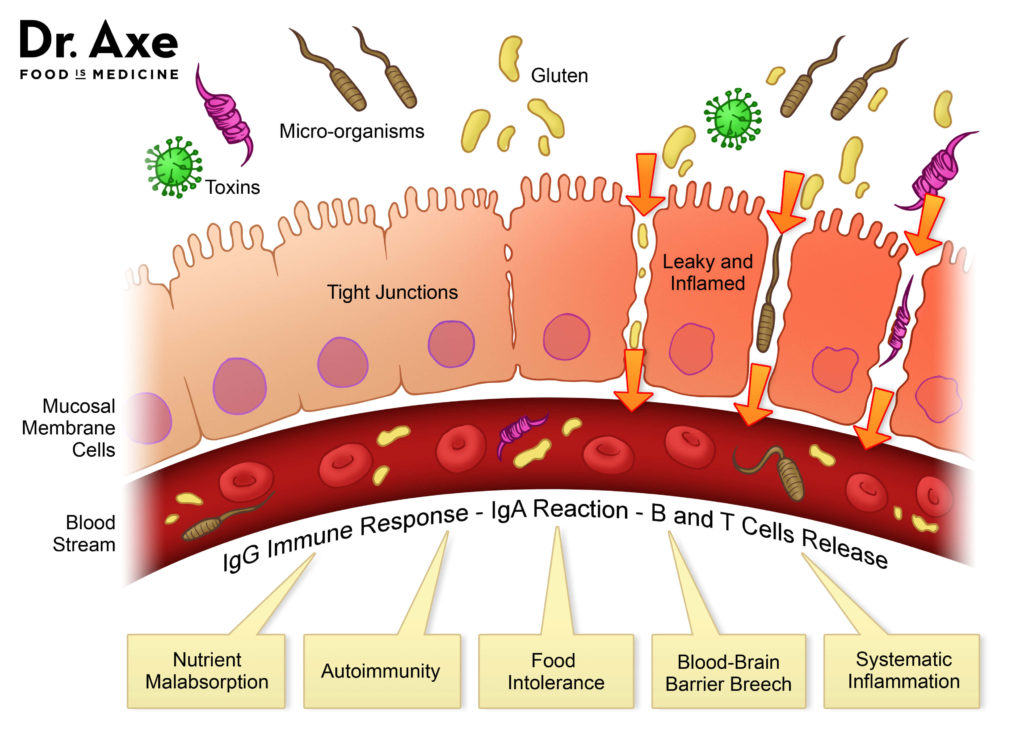
The gut barrier function serves as an interface between the person and their external environment. About 70% of the entire immune system resides in the GI tract2, and is on high alert when there are breaches in the gut barrier as a result of leaky gut or damage to the cells. An antigen is defined as a toxin or other foreign substance that induces an immune response in the body, especially the production of antibodies. This picture from Dr. Josh Axe, DC, shows the breach of the barrier and entrance of toxic antigenic substances such as unwelcome food proteins, bacteria and bacterial toxins into the circulation, triggering an antibody immune response. Once the immune system is triggered, the inflammatory process will be engaged. Prolonged inflammatory responses can further promote leaky gut.
How leaky gut affects health
With the passage of antigens into the body, the immune surveillance system sometimes views these molecules as invasive and a battle begins. Leaky gut can affect the whole body as demonstrated in this picture from Dr. Josh Axe, DC:
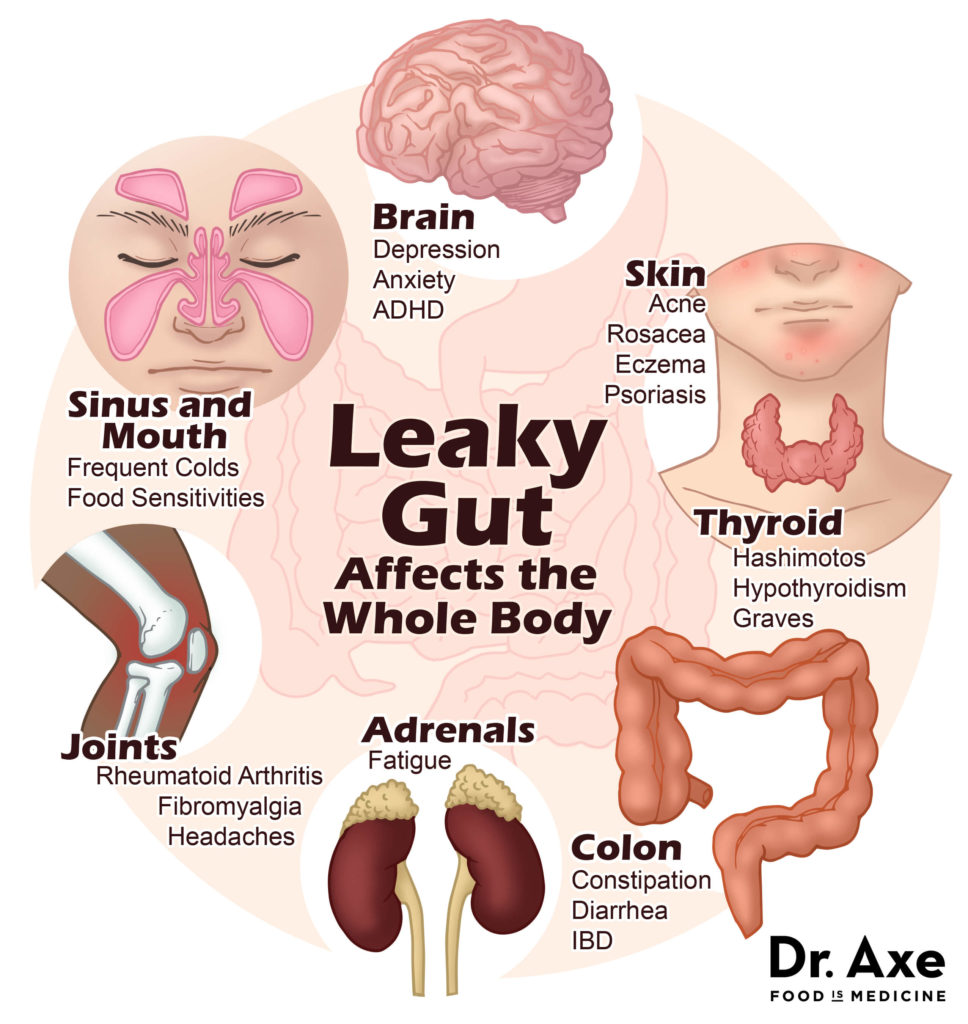
Basically, once the antigenic substance gets into the bloodstream, it can travel to anywhere in the body and create an inflammatory response. Multiple systems can be impacted leading to symptoms and conditions. Dr. Jill Carnahan, MD discusses how inflammation is a trigger for leaky gut and how this inflammatory process can manifest in different parts of the body, ultimately leading to autoimmune and other diseases.
How does leaky gut affect autoimmune disorders?
The theory around the development of autoimmune disease involves a trigger, increased gut permeability, and genetic susceptibility to that disease3. While there is not much we can do to change our genetics, we can make choices to avoid certain triggers, as well as do things that protect the integrity of our gut.
Celiac Disease (CD) is a good example of the autoimmune model. Patients who have CD have a genetic predisposition to this disease, possessing genes HLADQ2 and/or HLADQ8. Testing for these genes does exist through most conventional labs. People with these genes happen to secrete more zonulin which creates leaky gut. Zonulin is responsible for the opening of the tight junctions between the intestinal cells, and prolonged release of zonulin results in tight junctions that remain open for too long. When these people also eat gluten, excess gluten passes between the cells and the immune system flags the gluten as an antigen. The immune system then launches an attack on the “invader” and the result is destruction of the cells of the small intestine. The immune system is given a signal to attack itself. As long as the trigger (gluten) and the intestinal permeability continue, the immune system will continue to attack and destroy. For those who are scientifically-minded or like to see a visual representation of this process, a great article was published in Scientific American and written by Dr. Alessio Fasano, MD describing this connection. Once gluten is removed, the autoimmune attack on the intestinal cells ceases. When the GI system itself is the target of autoimmunity, as with such diseases as Crohn’s or Celiac, the intestinal destruction can further perpetuate the permeability issue, a vicious cycle.
Dr. Fasano makes another fascinating observation in the article referenced above about the connection with our bacteria and how they influence genetic expression: “Apparently they can also influence which genes in their hosts are active at any given time. Hence, a person whose immune system has managed to tolerate gluten for many years might suddenly lose tolerance if the microbiome changes in a way that causes formerly quiet susceptibility genes to become active. If this idea is correct, celiac disease might one day be prevented or treated by ingestion of selected helpful microbes, or ‘probiotics’.” There is more discussion on this topic in the “Repopulate” phase of the 5R approach.
The model described for the development of CD is thought to be the process that underlies all autoimmune disease, with different genes and triggers for different diseases. Some genes and triggers have not yet been discovered for many autoimmune diseases. They are all thought to begin with a leaky gut3. So regardless of whether triggers and genetics have been discovered for specific presentations of autoimmune disease, we already have tools to help with gut repair and strengthening to help heal them.
What causes leaky gut?
Dr. Alessio Fasano, MD is part of the team responsible for discovering the protein zonulin. In Dr. Fasano’s research, it was found that gluten and bacteria are the most potent stimulators of zonulin release. 1 Does this mean that gluten causes leaky gut in everyone? The answer is no; although it does promote tight junction opening in everyone, in healthy patients, this is a transient process and the tight junctions close in a timely manner. In an article on zonulin and leaky gut, however, Dr. Jill Carnahan, MD suggests that, “100% of patients with autoimmune disease or leaky gut could potentially benefit from a gluten-free diet.”
There are many other factors that contribute to leaky gut. Minimizing these factors ultimately results in healing of leaky gut. Some of these factors include eliminating:
- NSAIDs (non-steroidal anti-inflammatory drugs): In this interview, Dr. Fasano describes the connection with prolonged use of NSAIDs and the development of leaky gut, explaining that these drugs deplete the protective mucous layer. Instead of NSAIDs for pain management, consider natural choices. Dr. Mark Hyman, MD suggests anti-inflammatory herbs and supplements such as curcumin (from turmeric), boswellia, ginger and fish oil.
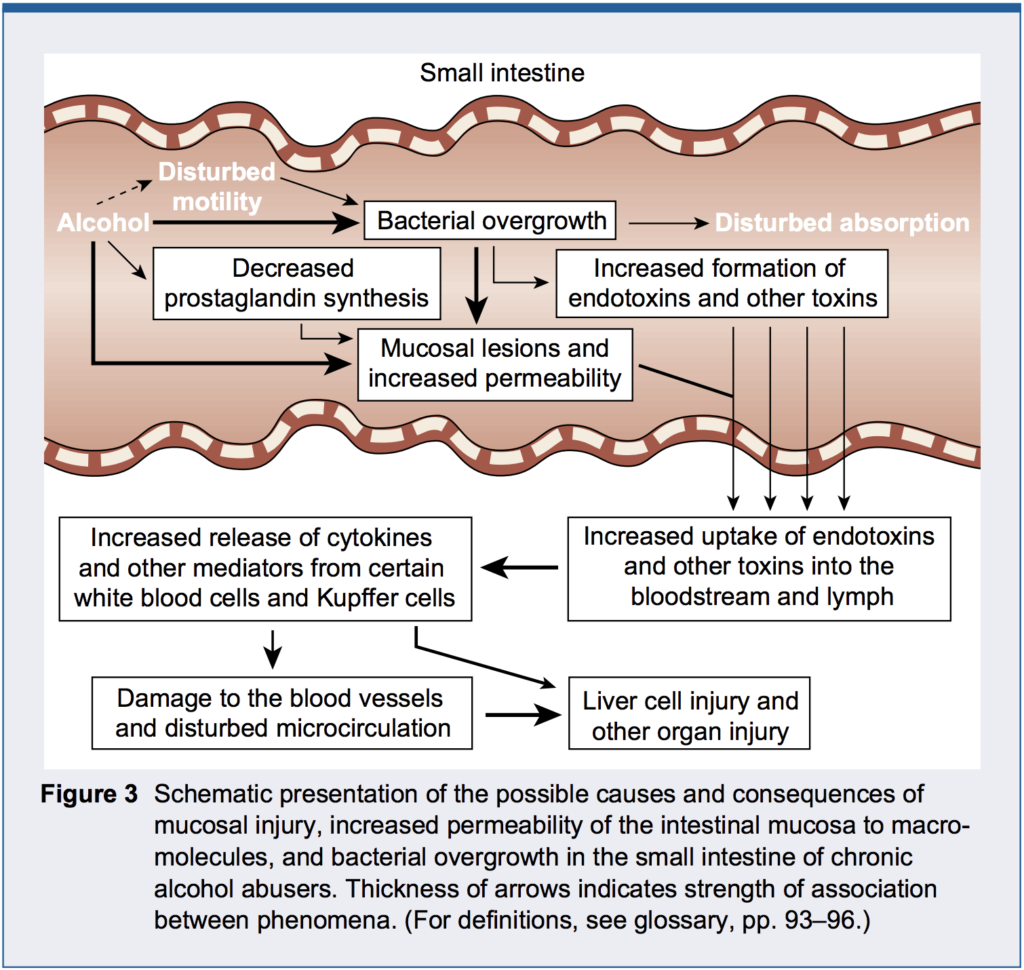
- Alcohol: As shown in the diagram below, alcohol leads to bacterial overgrowth, malabsorption and intestinal permeability in the small intestine. (Note the paper this diagram was pulled from also discusses the detrimental effect of alcohol on multiple organs of the GI tract including the esophagus, stomach and large intestine).
- Food allergies or sensitivities: The removal of these are discussed in the “Remove” phase of the 5R approach.
- Excessive sugar intake: Specifically, fructose, was shown to increase permeability in rodent studies.4 Fructose in the form of high fructose corn syrup is added to a lot of processed foods, which is why it important to read labels and stick to foods in their whole, unprocessed form.
- Radiation and chemotherapy: Due to the aggressive nature of these treatments used for cancer and other diseases, it is not surprising that they may damage the GI tract leading to permeability. Cancer centers that include a functional medicine staff realize the benefit of treating with gut repair substances.5,6
- Infectious organisms and dysbiosis: The importance of a healthy balance of organisms in our gut is the topic of discussion in the “Repopulate” phase of the 5R approach and the removal of infectious organisms is discussed in the “Remove” phase. The gut becomes a battle ground between an infectious organism and the immune system, with destruction of tissue and leaky gut as the collateral damage. Other organisms, considered opportunistic organisms, take their “opportunity” to overgrow when the normal defenses are down. Dr. Amy Myers, MD describes Candida yeast overgrowth as contributing to leaky gut. In addition to yeast overgrowth, Dr. Doni Wilson adds that bacterial dysbiosis and small intestinal bacterial overgrowth (SIBO) can also contribute to leaky gut.
- Systemic inflammation: Managing systemic inflammation with and anti-inflammatory lifestyle is key, as the circulating cytokines (inflammatory molecules) can perpetuate leaky gut.7 Leaky gut can trigger systemic inflammation and be a consequence of systemic inflammation- a vicious cycle.
- Nutrient deficiencies: Deficiencies in vitamin A, vitamin D and zinc have been associated with leaky gut.4,8,9
- Stress: The effect of stress on the gut is discussed in great detail in the “Rebalance” phase of the 5R approach.
- Prolonged, strenuous exercise: Athletes exposed to high-intensity exercise can have increased intestinal permeability.10 Sticking to a moderate-intensity movement program has multiple health benefits. For those who love high-intensity exercise, special attention should be paid to ongoing support of gut and immune health.
What can I do to heal a leaky gut?
Healing a leaky gut involves two things: decreasing causes (listed above) and increasing things that are reparative (listed below). If you think about a faucet leaking into a sink, and then overflowing, you have a few choices: you can simply turn off the faucet to prevent further overflow, and clean it up; or you can start cleaning it up while the faucet is still running, which will keep you cleaning forever! Using this analogy, if you do not decrease the causes of leaky gut, the gut will continue to be permeable and the immune system will continue to attack. But if you decrease the causes and stop that overflow, the body will have a chance to recover, without being under a constant barrage of insult.
When asked how long it takes to heal the gut, Dr. Amy Myers, MD mentions that it varies from person to person, but if following her gut repair program, it is about a three-month process. Dr. Doni Wilson, ND says three to six months, and beyond. She continues to support the healing of her leaky gut daily. She says, “I recommend that you do the same, because no matter how careful we are to avoid the causes, many daily activities and exposures can add up to a recurrence of leaky gut.”
The 5Rs as a gut-healing protocol overall
There are 5 “Rs” in the 5Rs program. They are Remove, Replace, Repair, Repopulate, Rebalance. The ‘remove’ phase involves removing triggers and things that may potentially cause leaky gut. The ‘replace’ phase involves adding or replacing things that help with digestion – digestive enzymes, for example, where undigested food can be an irritant to the gut lining, as well as substrate for the immune system to attack if the undigested food leaks through. In the ‘repopulate’ phase, probiotics are used, which can have a beneficial impact on the lining of the GI tract by regulating the immune response, thus toning down inflammation and allowing for repair. Probiotics and prebiotics also play a key role in feeding a healthy microbiome, which is the symbiotic environment of bacteria in our gut that holds the key to many health processes. The fifth phase of the 5Rs, the ‘rebalance’ phase, involves managing other lifestyle aspects that can negatively impact the gut lining, like stress.
More examples of leaky gut-healing protocols
When it comes to GI repair, there are multiple aspects to consider to heal the gut. There are substances that are nutritive and regenerative to the cells that line the gut, substances that have mucilaginous and thus soothing properties, substances with anti-inflammatory properties and so on. All of these properties are helpful. Many supplement companies have designed products that are comprehensive, so they can deliver many of these ingredients together in one product.
These substances should be vetted first through a functional medicine practitioner who can tailor these to the specific needs of the patient since not all are necessary for beneficial results, and some may be contraindicated for certain patients. Dr. Doni Wilson, ND writes a great article covering the top 16 supplements, nutrients and herbs she uses to heal leaky gut, which includes, for each supplement, who should avoid it. She breaks down the supplements into 3 categories: supplements that help with digesting food, supplements that help heal the intestinal lining, and supplements that balance the bacteria in the gut.
Functional medicine practitioners vary in their approach, but for the most part share similar protocols when it comes to leaky gut supplements. Dr. Jill Carnahan, MD gives some examples of supplements she uses with patients in her practice to heal leaky gut.
Summary of common ingredients used in leaky gut formulas:
Ingredient | Function | Example Daily Dosage |
| Glutamine | Intestinal cell support | 500 mg-10 grams |
| Zinc Carnosine | Anti-ulcerative, immune support | 25-75 mg |
| N-Acetyl Glucosamine | Intestinal cell support | 100-2000 mg |
| Aloe Vera | Mucilaginous, soothing | 300 mg |
| Slippery Elm | Mucilaginous, soothing | 200 mg |
| Marshmallow root | Mucilaginous, soothing | 100 mg |
| Deglycyrrhizinated Licorice (DGL) | Mucilaginous, soothing, anti-ulcerative | 400- 1800mg |
| Quercetin | Anti-inflammatory | 100 mg- 6 g |
| MSM (Methyl Sulfonyl Methane) | Anti-inflammatory | 100-250 mg |
| Turmeric (Curcumin) | Anti-inflammatory | 250-500 mg |
| Fish oil | Anti-inflammatory | 2-4 g |
| Vitamin A | Immune support | 2000 IU |
| Vitamin D | Immune support | 1000 IU minimum |
| Probiotics | Immune support | 20-40 billion units, or higher |
| Colostrum | Immune support, tissue repair | 1 g |
| Butyric Acid | Intestinal cell support | 100 mg |
- Glutamine: Glutamine, or L-glutamine is an amino acid that serves as the primary fuel source for intestinal cells.11 Foods containing glutamine, include bone broth, grass-fed dairy and meats, and plants such as cabbage and asparagus. Sometimes larger doses of a supplement are recommended, making capsules cumbersome to achieve the desired dose. In this case, a powdered form mixed in a liquid may be easier to reach the desired dosage. Dr. Josh Axe, DC has an entire article on glutamine if you are interested in learning more.
- Zinc carnosine: Zinc is anti-ulcerative and can protect the mucosal lining against NSAID-induced damage.12
- N-Acetyl Glucosamine: This substance is used to make support structures, called glycosaminoglycans in the intestinal cells.
- Aloe, marshmallow root, okra, cat’s claw, slippery elm: These herbs have mucilaginous properties, meaning they coat and soothe inflamed, injured tissue. They enhance normal mucosal secretions which form part of the protective mucous barrier of the GI tract.
- DGL: Deglycyrrhizinated licorice is a form of licorice that has the glycyrrhizin component removed. This particular constituent can cause elevated blood pressure when taken long-term. Being that such large amounts of DGL are encouraged for tissue repair and protecting the mucous lining, it is important to have the glycyrrhizin component removed. This supplement comes in a few different forms. A convenient form is in wafer form where you can dissolve several of these in your mouth throughout the day. It is also included in a lot of GI repair formulas as capsules or powder.
- Quercetin: This plant flavonoid naturally occurs in apples, onions and garlic. It stabilizes mast cells, which release histamine that promotes inflammation. It is best used in powdered form.
- Methyl sulfonyl methane (MSM): This is used as connective tissue support to promote structural repair and integrity. It is also anti-inflammatory.
- Turmeric (Curcumin): Turmeric is the yellow spice that most of us have in our spice cabinets. The root itself looks very similar to ginger root, but when you cut it open, you can see that bright yellow pigment. Both turmeric and ginger possess anti-inflammatory properties. Eating these as spices in dishes is great, but some people may also choose to supplement. In addition to its benefit for the gut, Dr. Josh Axe, DC describes the numerous other benefits for the body.
- Fish oil: Cold water fish is high in omega-3 fatty acids, which are anti-inflammatory. It can reduce systemic inflammation which is a cause of leaky gut. Many people choose to take a fish oil supplement that contains both eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), the two fatty acids that have potent anti-inflammatory activity. Choose a clean source that is tested for mercury.
- Vitamins A, D: As mentioned in the causes of leaky gut section, deficiencies of vitamins A and D can be associated with leaky gut.4 It is best to test vitamin D levels and dose with D3 accordingly.
- Probiotics: Beneficial bacteria support the gut barrier and microbiome both directly and indirectly. Probiotics are discussed in detail in the “Repopulate” phase of the 5R approach. Generally, a mixed strain/species product is recommended.
- Colostrum: Colostrum is produced by mothers in milk for their babies. It can heal repaired gastrointestinal tissue. Colostrum and its constituents lactoferrin and IgG can support immune defenses. Supplemental colostrum comes from a bovine source typically.
- Butyric Acid: Colon cells utilize butyric acid as a fuel source for regeneration and repair. It is a short chain fatty acid produced when the bacteria of the gut ferment fiber.
Many comprehensive GI reparative formulas include other ingredients that serve various roles. The ones mentioned here are some of the most common leaky gut substances utilized by functional medicine practitioners.
(Information from this section was gathered from various professional line supplemental product data sheets that are fully referenced as well as research articles. Dosages were gathered from these product data sheets as well as websites from doctors offering dosages and a functional medicine textbook13. Please note, these dosages in the chart serve as an example and actual doses prescribed by a functional medicine practitioner can vary widely compared to what is listed here.)
Testing for leaky gut
There are a few different types of tests for leaky gut, but many clinicians treat empirically, meaning, they assume the gut is already in disrepair based on the presentation of symptoms, and employ strategies for prevention and repair anyway. Dr. Josh Axe explains different tests for leaky gut.
The lactulose/mannitol absorption test is the gold standard test for intestinal permeability. It involves drinking a solution of the sugars lactulose and mannitol, then measuring their levels in the urine. Lactulose is a larger molecule that should not pass between the cells of the intestinal lining. If it does pass through, it will eventually be picked up by the blood stream and transported to the kidneys and end up in the urine. High lactulose levels in the urine suggests that it passed through the gut, and the only way that large of a molecule can pass through, is if the gut is hyperpermeable, or leaky. Currently, Doctors Data offers the Intestinal Permeability test and Genova Diagnostics offers the Intestinal Permeability Assessment.
As mentioned earlier, zonulin is a novel biomarker that was discovered in the early 2000s and tests have recently become commercially available. Zonulin can be measured both in the stool or blood. The companies that are currently offering zonulin tests include:
- Cyrex Labs Array 2- Intestinal Antigenic Permeability Screen
- Doctors Data Zonulin
- Dunwoody Labs Advanced Intestinal Barrier Assessment
- Genova Diagnostics Zonulin offered as an add-on test to other profiles
- Salveo Diagnostics Zonulin
Conclusion
In a nutshell, the entire 5R program serves to repair a leaky gut. The steps don’t have to be done in sequence. They can be simultaneous or one step at a time. The approach may be different depending on the patient. The important thing to remember is to be mindful of minimizing causes and triggers of leaky gut, and to increase those things that will contribute to a healthy gut barrier. Nobody is perfect and adhering to a strict regimen can feel limiting at times. The goal is not to be so rigid that it robs you of your joy. It is important, however, to do enough initially that tips the balance in the direction of healing. Then, once evidence of that initial healing happens, it can be very motivating to continue on a healthy path. As the body heals and becomes more resilient, it will better be able to handle previous insults. The goal is to continue to make healthy choices most of the time for the long-term, and to not risk gut compromise.
References:
Fasano A. Zonulin, regulation of tight junctions, and autoimmune diseases. Annals of the New York Academy of Sciences. 2012;1258(1):25-33. doi:10.1111/j.1749-6632.2012.06538.x.
Vighi G, Marcucci F, Sensi L, Di Cara G, Frati F. Allergy and the gastrointestinal system. Clinical and Experimental Immunology. 2008;153(Suppl 1):3-6. doi:10.1111/j.1365-2249.2008.03713.x.
Arrieta MC, Bistritz L, Meddings JB. Alterations in intestinal permeability. Gut. 2006;55(10):1512-1520. doi:10.1136/gut.2005.085373.
Bischoff SC, Barbara G, Buurman W, et al. Intestinal permeability – a new target for disease prevention and therapy. BMC Gastroenterology. 2014;14:189. doi:10.1186/s12876-014-0189-7.
Nejdfors P, Ekelund M, Weström BR, Willén R, Jeppsson B. Intestinal permeability in humans is increased after radiation therapy. Dis Colon Rectum. 2000 Nov;43(11):1582-1587; discussion 1587-8.
Melichar B, Kohout P, Brátová M, Solichová D, Králícková P, Zadák Z. Intestinal permeability in patients with chemotherapy-induced stomatitis. J Cancer Res Clin Oncol. 2001 May;127(5):314-8.
Hietbrink, F, et. al. Systemic inflammation increases intestinal permeability during experimental human endotoxemia. Shock. 2009 Oct; 32(4):374-378. doi: 10.1097/SHK.0b013e3181a2bcd6
Lima AAM, Soares AM, Lima NL, et al. Vitamin A supplementation effects on intestinal barrier function, growth, total parasitic and specific Giardia spp. infections in Brazilian children: a prospective randomized, double-blind, placebo-controlled trial. Journal of pediatric gastroenterology and nutrition. 2010;50(3):309-315. doi:10.1097/MPG.0b013e3181a96489.
Skrovanek S, DiGuilio K, Bailey R, et al. Zinc and gastrointestinal disease. World Journal of Gastrointestinal Pathophysiology. 2014;5(4):496-513. doi:10.4291/wjgp.v5.i4.496.
Clark A, Mach N. Exercise-induced stress behavior, gut-microbiota-brain axis and diet: a systematic review for athletes. Journal of the International Society of Sports Nutrition.2016; 13:43. DOI: 10.1186/s12970-016-0155-6
Rapin JR, Wiernsperger N. Possible Links between Intestinal Permeablity and Food Processing: A Potential Therapeutic Niche for Glutamine. Clinics. 2010;65(6):635-643. doi:10.1590/S1807-59322010000600012.
Mahmood A, FitzGerald AJ, Marchbank T, et al. Zinc carnosine, a health food supplement that stabilises small bowel integrity and stimulates gut repair processes. Gut. 2007;56(2):168-175. doi:10.1136/gut.2006.099929.
Guilliams, Thomas. Functional Strategies for the Management of Gastrointestinal Disorders. Point Institute. 2016. pp 153-160.



